Every year significantly more people die during the winter months than at other times of the year, and recently we have seen huge variability in ‘excess winter deaths’, potentially impacted by the severity of the flu.
3 October 2019
In this edition of VitaMins Health we explore the subject of flu.
With annual volatility in death rates being largely driven by the level of excess winter deaths and as many as a third caused by respiratory diseases, can we use an understanding of influenza patterns to help predict future events? And how much should annual fluctuations of data due to the effectiveness of a vaccine or the most prevalent flu strain affect long-term projections?
What is seasonal influenza?
Influenza is a virus which affects the respiratory system. It is usually non-life threatening, however, certain groups, such as the over 65s, under 5s, pregnant women and the severely obese are far more at risk of life-threatening complications. According to the Centers for Disease Control and Prevention (CDC) in the United States 70-90% of seasonal flu-related deaths occur in people over 65.
Most influenza infections occur during the winter due to a combination of factors, potentially including:
- A decline in ultraviolet (UV) radiation reducing the chances of the virus being killed by UV.
- Production of Vitamin D, vital for the immune system, decreasing due to the lack of sunlight.
- People staying indoors more , increasing the likelihood of transmission.
The two most common types of influenza virus which infect humans are known as A and B; with influenza A being more common and generally more severe. There are also many different subtypes of the virus; the two most prevalent subtypes of influenza A are called H1N1 and H3N2.
How does flu affect mortality?
Due to the nature of the global community, seasonal effects of influenza are similar across the Northern Hemisphere.
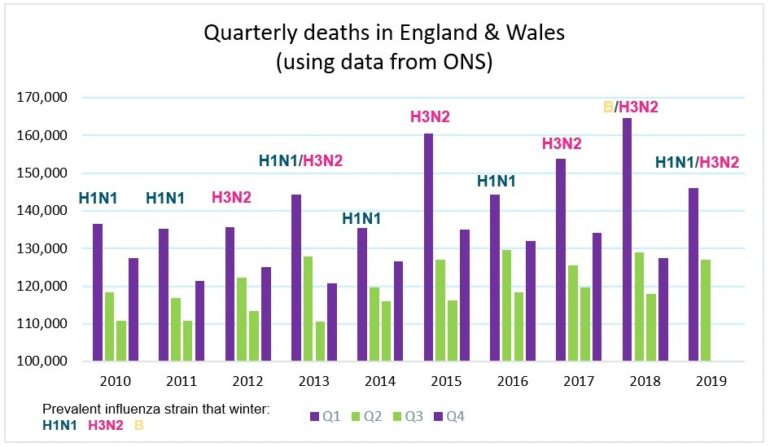
As an example, we highlight in the chart the number of deaths in England & Wales each quarter from 2010 to mid-2019. The purple bars represent winter deaths, showing a spike in deaths in the first quarter of each year.
Using data from Public Health England (PHE) we have overlaid which flu subtypes were most prevalent each year (by number of identified cases). H3N2 was dominant in the recent winters with the highest numbers of deaths, suggesting that H3N2 has recently been more life-threatening than H1N1. However, continual mutations of the virus mean this effect may well change over time.
The flu vaccine: choice of strains and the production process.
Each winter, various public health programs promote vaccination against influenza for at-risk groups. The vaccine is designed to combat the most prevalent strain of the virus that year. Due to rapid mutations of the influenza virus, the vaccine’s effectiveness will vary and likely decrease over time.
So how are vaccine strains chosen? Organizations around the world, such as the CDC in the US and PHE in the UK, collect data on circulating influenza strains and monitor the virus’ genome and structure. In February each year, the World Health Organization (WHO) decides which strains are most likely to be prevalent in the Northern Hemisphere next winter, based on information such as the strains currently prevalent in the Southern Hemisphere and those which have dominated in recent years (there is a similar process for the Southern Hemisphere in August). However, this estimate is not always correct; the high number of excess winter deaths in 2014-15 was widely attributed to a mis-match in the vaccine and the most prevalent flu strain.
The vaccine strains are chosen in February for the following winter because producing large quantities of influenza vaccine takes at least six months. The vaccine is typically made inside fertilized chicken eggs, one egg per vaccine dose, which is a very slow process.
The future of the flu
The impact of the flu on mortality will be largely dependent on the ability to vaccinate against it effectively. This has many challenges which various advances in treatment are trying to combat.
Universal vaccine
A universal vaccine is one that would protect an individual from all influenza viruses. There is currently no universal flu vaccine licensed for human use, however there are some promising drugs in clinical trials, although these are still at least 5 years away from commercial use.
Vaccine production
There are two newer production processes for creating the influenza vaccine: a cell-based method and a form of DNA manufacturing known as recombinant. Both methods are faster than the egg-based process, with recombinant being the fastest. Adopting these faster processes would allow the WHO to choose the influenza vaccine strains later, with a more accurate picture of the prevalent strains. This would increase vaccine efficacy and ultimately save lives.
Despite recombinant technology offering faster production, there remain some issues preventing its wide adoption: cost, a short shelf-life and insufficient infrastructure to mass-produce globally.
What does this mean for pension plans and insurers?
The number of deaths experienced in a country each year drives our best estimates for how long people will live both now and in the future. The relative number of deaths experienced in any particular year can be largely affected by the level of excess winter deaths, which in turn is driven by the most prevalent flu strain and the efficacy of that year’s vaccine. Monitoring common strains of flu in other parts of the world and advances in vaccine effectiveness could give early warnings to data effects that will feed into future models.
We should also be wary of models that are too sensitive to a single year’s experience data. How much should a mis-match in the most prevalent strain of influenza and the strain covered by that year’s vaccine really affect our long-term outlook on longevity improvements?
VitaMins Health: Getting clued up on flu
Download a print friendly version of this article.



