The provision of medical services has been significantly reduced in the face of the COVID-19 pandemic. What are the implications for mortality rates in the months ahead?
8 January 2021
During 2020 our blogs explored the emerging, and tragic, death toll arising from COVID-19, looking beyond the headline numbers seen in the daily news. These deaths are now sadly on the rise again and have understandably been the focus of a lot of media attention.
There has perhaps been less exploration of patterns in non COVID-19 deaths, and whether these have dropped (for example due to COVID-19 bringing forward by a few months deaths which may have otherwise occurred anyway) or increased (as a consequence of a potential ‘hidden’ cost of COVID-19). Many in the medical profession have expressed concerns about the consequences of the interruption and disruption to medical services during the pandemic.
The ‘missed’ deaths
During the first wave of the pandemic in the UK we saw considerable COVID-19 deaths during April and May – around 50,000 once we include all deaths where COVID-19 was mentioned on the death certificate. Note that this is higher than the figure quoted in government statistics which is limited to those who died within 28 days of a positive COVID-19 test (around 37,000 reported by the end of May).
At the same time as this wave of COVID-19 deaths, we also saw a marked rise in ‘non COVID-19’ deaths (i.e. deaths with no mention of COVID-19 on the death certificate). It has been suggested that this rise, contributing some 14,000 deaths above seasonal norms, is likely to have been a result of some combination of undiagnosed COVID-19 cases (particularly at the start of the pandemic), and preventable deaths as a result of delays in accessing medical services and/or treatment, and increased pressures on healthcare services, for example capacity in ICU beds.
Following the first wave, non COVID-19 deaths returned to close too, and often below, seasonal average levels for much of the rest of 2020. Whilst COVID-19 undoubtedly brought forward some deaths, notably amongst the frailest of our older generations, this is only part of the story. Many of those who died were not “at deaths door” prior to COVID-19. Strong concerns remain that there may be further rises in non-COVID-19 deaths in the short to medium term because of the disruption seen.
Impact of disruption on emergency admissions
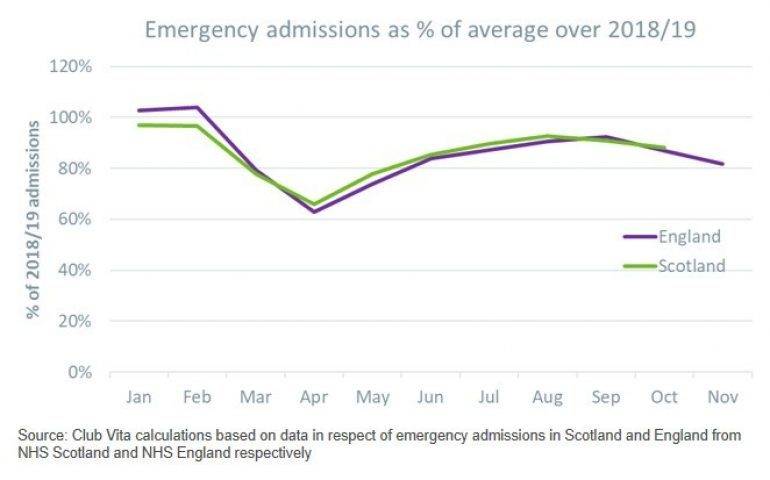
Concerns around the perceived risk of catching COVID-19, a wish to avoid ‘putting the NHS out’, and the general messaging of lockdowns and social distancing, have all contributed to significant falls in people seeking medical advice since March. Despite ongoing efforts by the NHS to encourage people to continue to seek medical attention, emergency admissions in England and Wales had not returned to normal by September, even before the second wave of infections.
For England emergency admissions in November 2020 were around 20% below the levels seen in November 2018 and 2019; similarly, by the end of October, emergency admissions in Scotland were c10% below 2018 and 2019 levels.
This fall in emergency admissions coincided with a rise in deaths occurring at home. The numbers of deaths from conditions that require timely treatment to avoid being fatal (such as diabetes, epilepsy and hypertensive disease) also remained higher than average during May and June. It has been suggested that these figures could be a consequence of delayed access to care.
Impact of disruption on detection, diagnosis and treatment
The reduced ‘demand’ for medical services from the public has been combined with reduced ‘supply’ afforded by the NHS. For example, GP surgeries have been restricted both in terms of numbers and capacity as a result of social distancing, particularly for face-to-face appointments. This disruption will impact on the ‘detection-diagnosis-treatment’ pathway, which is critical to avoiding premature mortality from heart disease/strokes, as well as the detection of cancers in their early, more treatable, stages.
Taking the cancer pathway as an example, we highlight below how each step – from the initial detection of a potential problem, through to diagnosis and treatment – has been impacted by COVID-19.
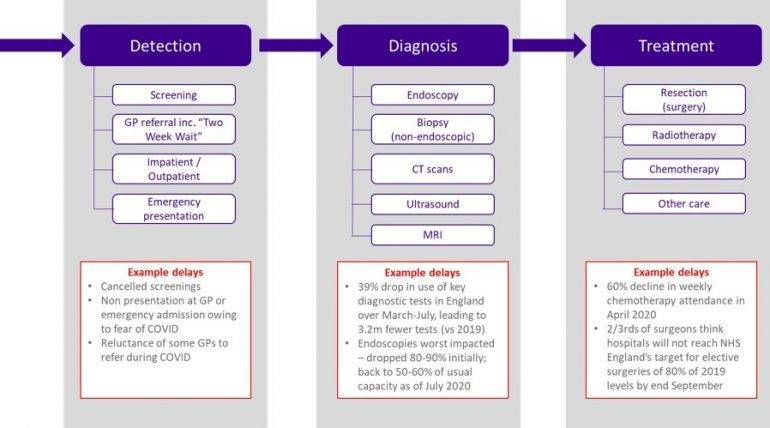
Prior to COVID-19, around 55% of cancers were diagnosed at Stage 1 or 2, with plans in place to increase this to 75% by 2028. As the stage of diagnosis makes a material difference to survival rates (e.g. one year survival rates for colorectal cancer are 96% when diagnosed at stage 1 and 46% when diagnosed at stage 4), it seems inevitable that the disruption to services will result in increased mortality rates from ‘preventable’ cancer deaths in the future.
The exact impact is difficult to estimate as we need to assess the impact of delays to each step from detection to diagnosis and eventual treatment. This is linked to how long the disruption lasts for (and so duration of second wave / success of the vaccine program) and the pace of any “catch-up” program the NHS is able to implement post COVID.
In addition, many of the patients who began treatment in 2020 will be using different treatment methods to mitigate COVID-19 risks (e.g. switching treatment to radiotherapy rather than surgery and making earlier use of stereotactic radiotherapy). The impact of these treatment changes will only be known in the months and years to come.
Impact on other services
Although we have focused on cancer pathways above, other treatment services have seen similar impacts, including those relating to heart disease and dementia (the other major causes of death at older ages).
Heart disease: Some 28,000 heart procedures had been postponed in England, while numbers attending A&E with suspected heart attacks also fell by 50% over March.
Dementia: Both primary care and specialist services to diagnose dementia have been impacted by COVID-19. Rates of dementia diagnosis have dipped, and concerns have been raised about the impact on undiagnosed dementia sufferers not being able to access the necessary interventions and subsequent support services.
Many dementia sufferers live in care homes, and so have experienced social isolation during the stringent lockdowns. Prolonged periods without visitors, or at best much reduced visiting, can be a significant factor in deterioration of their condition, as well as the increased stress and confusion that comes with changes to routines, staff wearing masks, inability to ‘walk about’ etc.
Combatting the disruption backlog
The widespread cancellation and postponement of treatments, combined with drops in diagnosis rates, has led to a substantial backlog as services begin to resume and people are encouraged to seek medical advice as necessary. Estimating the total impact of the disruption to services requires consideration of the scale of disruption to date, a view on how long it will continue, and the extent to which the developing winter wave of the pandemic will further disrupt services.
The NHS has been implementing the third phase of its response to COVID-19, seeking to accelerate the return to near-normal levels of non COVID-19 health services and make fullest use of the capacity available to clear some of this backlog before the anticipated winter demand pressures. Despite these efforts, with approximately four million people in England waiting for NHS treatment prior to the pandemic, it is likely that waiting times will get materially worse in the short-medium term. Recent developments with the new more infectious variant, and the tighter nationwide restrictions now in place, as well as the need to resource rollout of the vaccines, will further stretch limited resources.
Options to clear the backlog include:
- Making greater use of the private sector;
- Increasing hospital capacity by extending operative hours (although this has knock-on implications for medical and other staffing requirements); and
- Making extended use of, for example, the ‘Nightingale’ medical facilities.
Ultimately though, capacity has a human constraint with regards to the number of trained clinicians able to deliver the services, and so it will take many months, if not years, to clear the backlog.
Tragically it appears inevitable that we will be feeling the disruptive impact of the pandemic for many years to come.
Vitamins: Life on pause
Download a print friendly version of this article



